Classification of UTIs
UTIs are classified clinically (asymptomatic versus symptomatic), anatomically (cystitis versus pyelonephritis) and by incidence (single versus recurrent). Recurrent UTIs are often the result of:
- inadequate antimicrobial therapy
- non-compliance
- bacterial resistance
- host susceptibility
- factors contributing to urinary stasis.
Clinical signs and symptoms
The clinical presentation varies and is often non-specific, particularly in young infants. This makes early diagnosis and management of paediatric UTIs challenging. Therefore, UTIs should be suspected in every febrile infant until proven otherwise.
History-taking includes an antenatal history, along with a family history of urological abnormalities, especially VUR. A full voiding history should include frequency, urgency, stream, volume, suprapubic pain, dysuria, secondary enuresis and toileting practices. Other relevant history includes the amount of fluid intake and bowel habits. In younger children, carers may report non-specific symptoms such as lethargy, fever, vomiting, malaise, failure to thrive, irritability and offensive urine.
No physical sign is pathognomonic for a UTI. On examination, physicians should promptly assess if the patient appears ‘sick’ or ‘well’, and be suspicious of fever, hypertension, a palpable bladder, dribbling or straining, and loin or suprapubic tenderness. Although often unremarkable, physical examination should include assessment of the abdomen, external genitalia, lower limbs and hydration status. In rare instances, underlying conditions that contribute to UTIs, such as spina bifida, phimosis, labial adhesions or sexual abuse, may be present.
Investigations
Urine collection, urinalysis and cultures
Urine should be collected if there is an unexplained fever (>38°C) and/or symptoms suggestive of a UTI.7,15 Collection of uncontaminated urine samples can be challenging in infants and should be performed using one of these methods (Table 1):
- clean catch (CCU)
- mid-stream (MSU)
- catheterised specimen (CSU)
- suprapubic aspiration (SPA).
Bagged urine specimens are often contaminated. A negative sample may exclude a UTI, but all positive bagged urine results should be confirmed using a CCU, MSU, CSU or SPA sample before commencing treatment.16 Urine samples should be collected prior to antibiotic administration to prevent false negative results.
Urinalysis is a quick, non-invasive method to screen for UTIs. However, urinalysis alone is not sufficient to diagnose a UTI. Positive readings for nitrite (75% UTI probability) and leukocyte esterase (30% UTI probability) may suggest a UTI. Urinalysis has 82.5% sensitivity, 81.3% specificity, 33.9% positive predictive value and 97.6% negative predictive value.17 In febrile children, urinalysis can help to identify who should receive antibacterial treatment while cultures are pending.
Diagnosis
UTI diagnosis is based on clinical symptoms in association with a positive urine culture. The amount of bacterial growth required for a positive culture varies by age and method of urine collection (Table 1). Even though treatment may begin prior to receiving culture results, the causative organism and antibiotic sensitivity should be evaluated to formulate a targeted therapeutic regimen.
Urinary tract imaging
In most circumstances, urinary tract imaging is not recommended following the first UTI.15 Renal ultrasonography seldom provides information that alters management. Clinicians should be aware of the indications and limitations of urinary tract imaging and use clinical judgement when seeking further imaging. Table 2 summarises the indications, uses and limitations of common urinary tract imaging modalities.
Management of UTIs
Treatment and care involves good communication between healthcare professionals, children and carers. Gillick competent children should be involved in the management of their health.19 Figure 1 provides an algorithm for the routine medical management of paediatric UTIs.
Conservative management
A positive urine culture in the absence of clinical symptoms may indicate asymptomatic bacteriuria and does not warrant treatment or further investigation. For all children, general measures that improve hygiene, hydration and bowel habits are recommended.7,15
Medical management
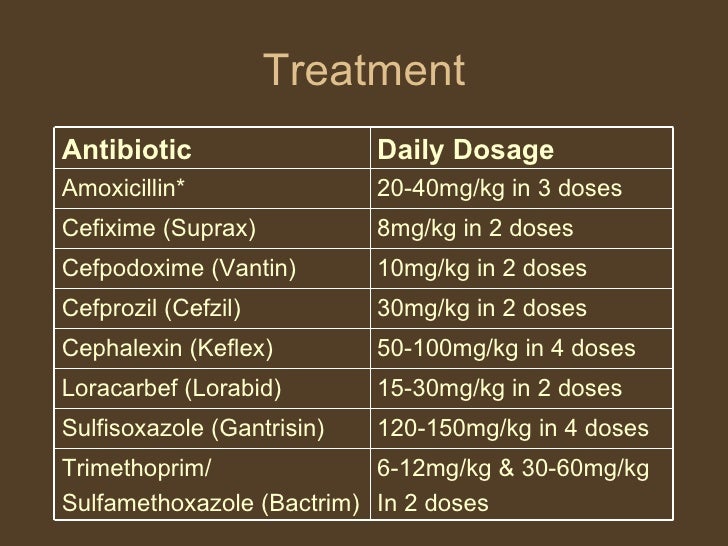
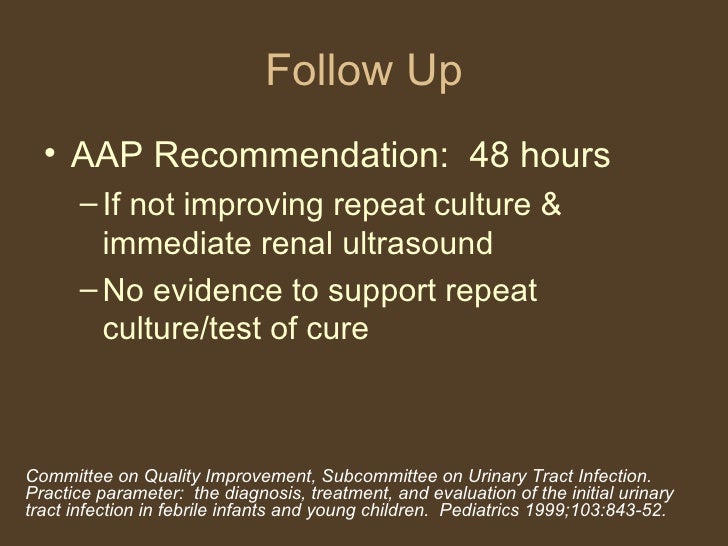
Treatment should be tailored to clinical severity and depends on the child’s age. Broad spectrum oral antibiotics will treat most uncomplicated UTIs. Comparatively, children with apparent sepsis, in shock and/or ❤ months of age should be treated aggressively with parenteral antibiotics and intravenous fluids. These patients should be referred to hospital for a full septic screen, including lumbar puncture and paediatric review.7,15 Antibiotic choice is governed by microbial sensitivities and local policies (Table 3, available online only). Every patient should be reassessed 48 hours after starting antibiotics, and treatment should be modified as per cultures and sensitivities. Empirical gentamicin therapy should not be used for longer than three days. If empirical therapy is still required, switching to ceftriaxone should be considered to reduce the risk of nephrotoxic and ototoxic side effects.20
Surgical management
Evidence suggests that boys have a 1% UTI risk in their first year, but this risk is reduced to 0.1% if they are circumcised.2Routine circumcision is not recommended, given that approximately 111 boys would need to be circumcised to prevent one UTI. However, having already had a first UTI in the first year of life confers further risk and circumcision may provide additional benefit, especially for those with recurrent UTI or grades III–V VUR.15 Prior to circumcision, hypospadias should be evaluated. Furthermore, surgical VUR correction should be considered only for persistent grade III–V VUR and/or failed continuous antibiotic coverage.15,21
Alternative management
The evidence indicates that cranberry concentrates effectively treat UTI symptoms in adults. However, there is no evidence to suggest that cranberry concentrate is therapeutic, prophylactic or reduces UTI symptoms in children, and is not recommended.22
Prevention and follow-up
According to Australian guidelines, antibiotic prophylaxis is not recommended for children after a first UTI.15 Instead, antibiotic prophylaxis should be considered for VUR grades III–V and/or complicated, recurrent UTIs. This decision should be made by a specialist or general practitioners specialising in paediatric care.1,23 When trialling antibiotic prophylaxis, continuation should be reviewed every six months. In addition, conservative measures such as increasing fluid intake, avoiding bubble baths, improving hygiene, and addressing constipation and dysfunctional voiding issues should be addressed to limit recurrence.24
Infants generally do not require follow-up if they have had asymptomatic bacteriuria or normal imaging. Children with recurrent UTIs should be assessed by a paediatrician and may require additional imaging, blood pressure monitoring and proteinuria assessment. Infants with impaired renal function or bilateral renal abnormalities require close paediatric involvement, annual blood pressure monitoring, renal imaging and renal function tests. It is import to note that any febrile event in these children needs to be investigated with urine cultures.7