Overview
Organophosphates are a common class of insecticides. But large doses of organophosphates can also harm people and other animals. Organophosphate poisoning can occur when you’re exposed to them for too long or at high levels.
Organophosphates are typically colorless-to-brown liquids at room temperature. Some may be unscented, while others have a fruit-like smell.
Researchers say as many as 25 million agricultural workers across the developing world have at least one episode of organophosphate poisoning per year. It’s being seen with more frequency in areas where there is limited access to insecticide safety gear, such as suits and breathing apparatuses.
Terrorist use of organophosphates is rare, but it has occurred. Sarin, an organophosphate poison, has been intentionally used twice in terrorist attacks in Japan.
What are the symptoms of organophosphate poisoning?
Organophosphate poisoning can be short- or long-term. It can be caused by large or small doses. The longer the exposure and the larger the dose, the more toxic the effects. Symptoms can occur within several minutes or hours of exposure.
Mild organophosphate exposure may cause:
- narrowed, pinpointed pupils
- impaired, blurry vision
- stinging eyes
- runny nose
- watery eyes
- excess saliva
- glassy eyes
- headache
- nausea
- muscle weakness
- muscle twitching
- agitation
Moderate signs of organophosphate exposure include:
- very narrowed pupils
- dizziness
- disorientation
- coughing and wheezing
- sneezing
- difficulty breathing
- drooling or excessive phlegm
- muscle twitching and tremors
- muscle weakness
- fatigue
- severe vomiting and diarrhea
- involuntary urination and defecation
Emergency signs of organophosphate poisoning include:
- very narrowed pupils
- confusion
- agitation
- convulsions
- excessive body secretions, including sweat, saliva, mucus, and tears
- irregular heartbeat
- collapse
- respiratory depression or arrest
- coma
What are the complications of organophosphate poisoning?
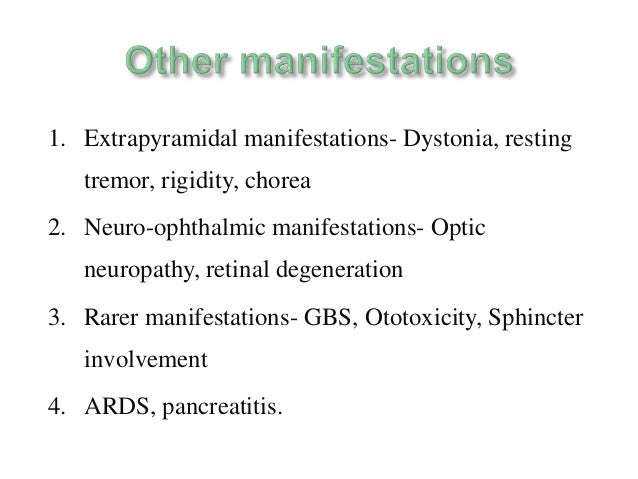
Organophosphate poisoning can cause several serious complications. These include:
- metabolic disorders, such as hyperglycemia (high blood sugar) and glycosuria (excess sugar in urine)
- diabetic ketoacidosis, in which your blood produces excess blood acids
- pancreatitis, or inflammation of the pancreas
- cancer
- neurological problems, such as muscle weakness and twitching, poor concentration, poor memory, and post-traumatic stress disorder
- fertility problems
- paralysis
Complications tend to become worse the longer and more intensely you are exposed to organophosphates.
What causes organophosphate poisoning?
The people most at-risk for unintentional organophosphate poisoning are those who live or work on or near farms. You can also get organophosphate poisoning by consuming contaminated food or water. The most common unintentional exposure routes are through breathing and contact with the skin.
People who intentionally expose themselves to organophosphates tend to inhale and ingest it. These concentrated, high doses are often fatal.
How is organophosphate poisoning diagnosed?
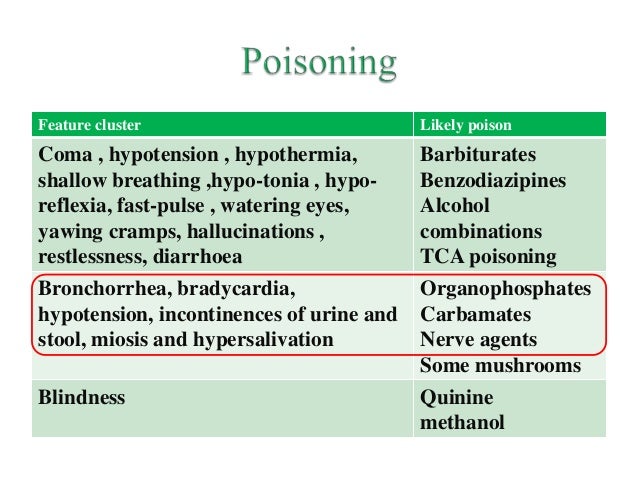
If you suspect you were exposed to some type of harmful chemical, your doctor will work to determine which is affecting you. There are subtle differences between the effects of various types of poisons. Organophosphate poisoning is distinguished from other types of poisoning by a very fast onset of symptoms.
If you have symptoms of organophosphate poisoning, your doctor try to determine how severely you were exposed. They will do this through blood and urine tests.
How is organophosphate poisoning treated?
The first goal of treating emergency cases is stabilization. Emergency care workers will:
- decontaminate your body to prevent further exposure
- stabilize your breathing
- use intravenous fluids to flush your system of toxins
In non-emergency cases, healthcare providers will still administer some supportive therapy. They’ll pay close attention to your breathing. Respiratory function is weakened by organophosphate exposure.
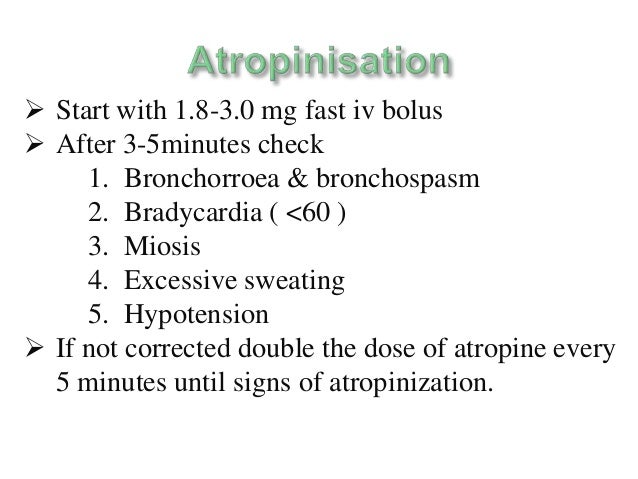
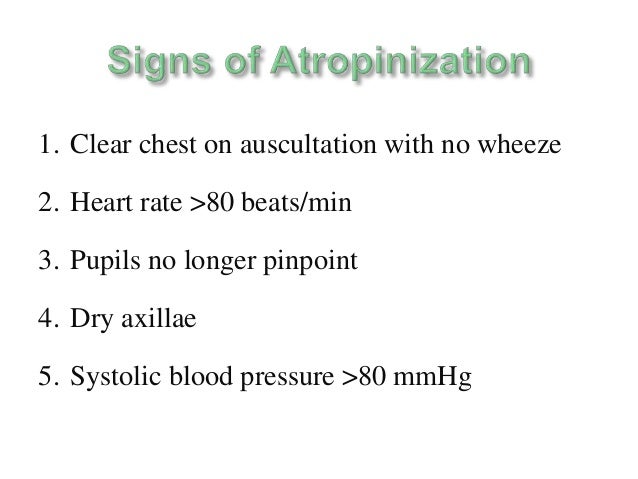
Doctors may administer a drug called atropine to stabilize your breathing. They may also administer pralidoxime, which can help relieve neuromuscular problems. In severe cases, doctors often prescribe benzodiazepines to prevent or stop seizures.
If you have been exposed to organophosphates in small doses and don’t need to be hospitalized, you may administer a low dose of atropine to yourself using a commercially prepared injection:
| Age and weight | Dose |
| adults and children who weigh more than 90 pounds (41 kilograms) | 2 milligrams (mg) |
| children weighing 42 to 90 pounds (19 to 41 kilograms) | 1 mg |
| children weighing less than 42 pounds (19 kilograms) | 0.5 mg |
An injection of 10 mg diazepam is recommended for people exposed to chemical attacks of organophosphates.
What’s the outlook for organophosphate poisoning?
Organophosphate poisoning is a serious medical condition, no matter how small the dose. Long, high-intensity exposures are the most concerning. See a doctor right away if you believe you’ve been exposed to organophosphate chemicals. Seek emergency treatment immediately if you’re displaying severe signs of poisoning.
Call 911 or seek emergency medical attention right away if you or someone you know has attempted suicide with organophosphates or any other method. If you or someone you know is thinking about suicide, call the National Suicide Prevention Lifeline at 1-800-273-8255. If you can safely prevent a person from attempting suicide, do so and take them to a hospital right away.
**************************************************************************









































![ï A newer model, the ATNAA (Antidote
Treatment Nerve Agent Auto-Injector),[1]
ï Has atropine and the pralidoxime in one
sy...](https://image.slidesharecdn.com/organophosphoruspoisoning-151107172353-lva1-app6892/95/organophosphorus-poisoning-53-638.jpg?cb=1446918010)




*****************************************************************************