INTRODUCTION
Late-onset neonatal sepsis (LOS) remains an important cause of death, morbidity and long-term complications among premature infants, which are associated with prolonged hospital stay and increased health-care costs.1It is of great interest to know the incidence and the strategies that are effective for preventing LOS in neonatal intensive care units (NICUs).
The most common infections seen in neonates are central line-associated bloodstream infections (CA-BSIs), which substantially contribute to the burden and cost of neonatal care.5 One proposed approach to achieve low CA-BSI rates is implementation of catheter care bundles.
Late-onset sepsis in premature infants is a major cause of morbidity, mortality, and increased medical costs.
Risk factors include low birth weight, low gestational age, previous antimicrobial exposure, poor hand hygiene, and central venous catheters.
Methods studied to prevent late-onset sepsis include early feedings, immune globulin administration, prophylactic antimicrobial administration, and improved hand hygiene.
Late-onset sepsis (LOS) is a common complication of prolonged admission to the neonatal intensive care unit (NICU) following preterm birth.
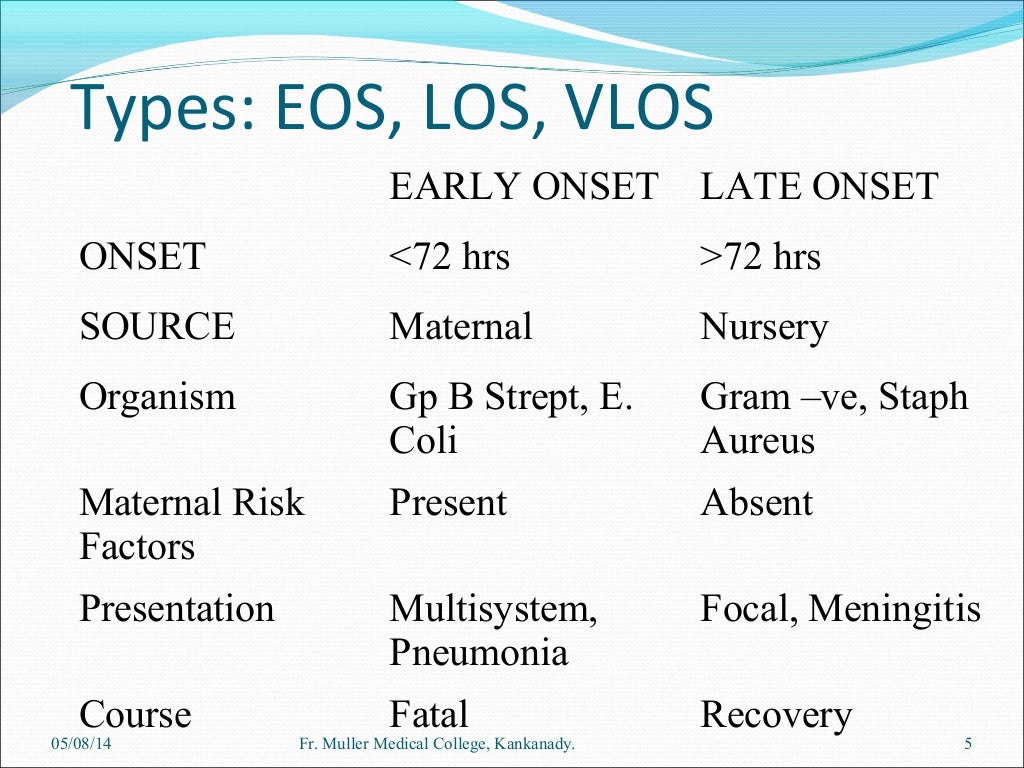
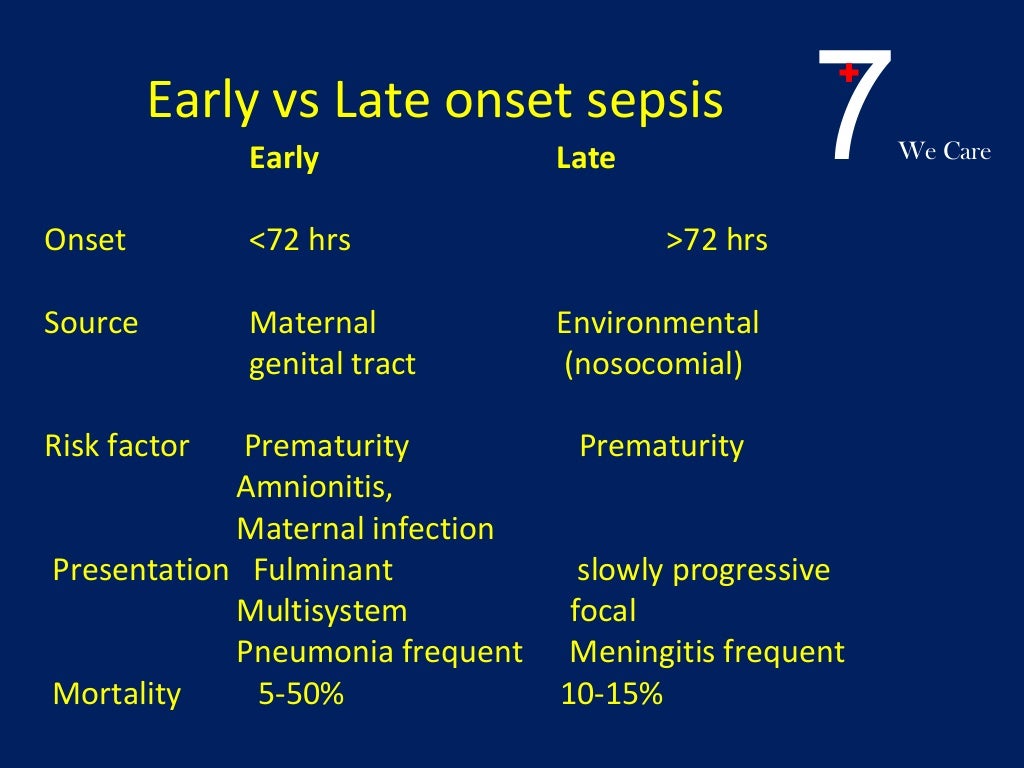
Neonatal sepsis is categorized as either early-onset (EOS) or LOS. EOS, often due to group B Streptococci or Escherichia coli, occurs in the first 3 days of life and is associated with prolonged rupture of membranes, maternal colonization with group B Streptococci, and prematurity .
LOS occurs after the third day of life and, among premature infants, is most often caused by Gram-positive organisms.
The causative organism in LOS is an important predictor of overall outcome. Gram-positive organisms account for 45–77% of infections.
Of the Gram-positive organisms, coagulase-negative Staphylococci are the most prevalent.
Late-onset sepsis (LOS) in preterm infants is a leading cause of mortality and morbidity. Timely recognition and initiation of antibiotics are important factors for improved outcomes.
Identification of risk factors could allow selection of infants at an increased risk for LOS.
******************************************************************
Neonatal Sepsis
II. Definitions
- Neonatal Sepsis
- Invasive infection in first 30 days of life
- Early onset Sepsis
- Intrapartum infection within first 72 hours of life
- Neonatal Sepsis within the first week of life
- Late onset Sepsis
- Neonatal Sepsis onset at 7 to 30 days of life
- Some studies define late onset as everything after the first 72 hours
- Results from postnatal infections
III. Epidemiology
- Incidence: 1-2 cases per 1000 live births
- Meningitis occurs in one third of Sepsis cases
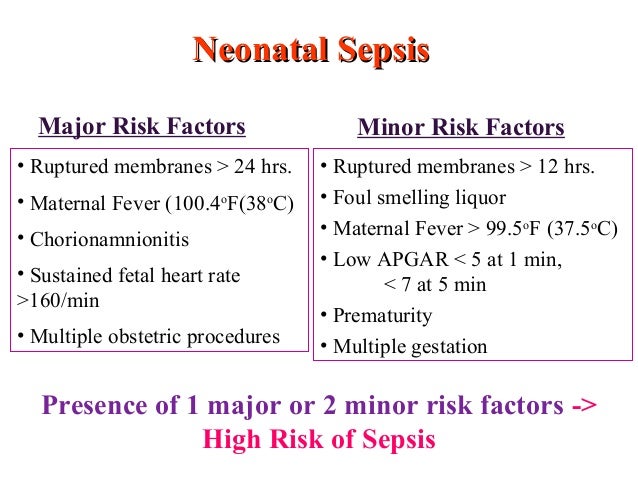
IV. Risk Factors: Early onset Sepsis
- Major
- Maternal prolonged Rupture of Membranes >18-24 hours
- Intrapartum Maternal Fever >38 C (>100.4 F)
- Chorioamnionitis
- Sustained Fetal Tachycardia >160 beats per minute
- Minor
- Intrapartum Maternal Fever >37.5 C (>99.5 F)
- Twin Gestation (or other Multiple Gestation)
- Premature Infant (<37 weeks)
- Maternal Leukocytosis (White Blood Cell Count >15,000)
- Maternal Urinary Tract Infection
- Prolonged Rupture of Membranes > 12 hours
- Tachypnea (<1 hour)
- Maternal Group B Streptococcus Colonization
- Low APGAR (<5 at 1 minute)
- Low birth weight (<1500 grams)
- Foul lochia
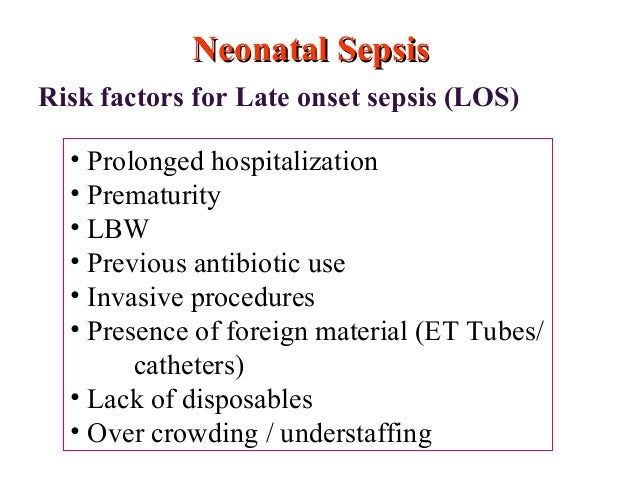
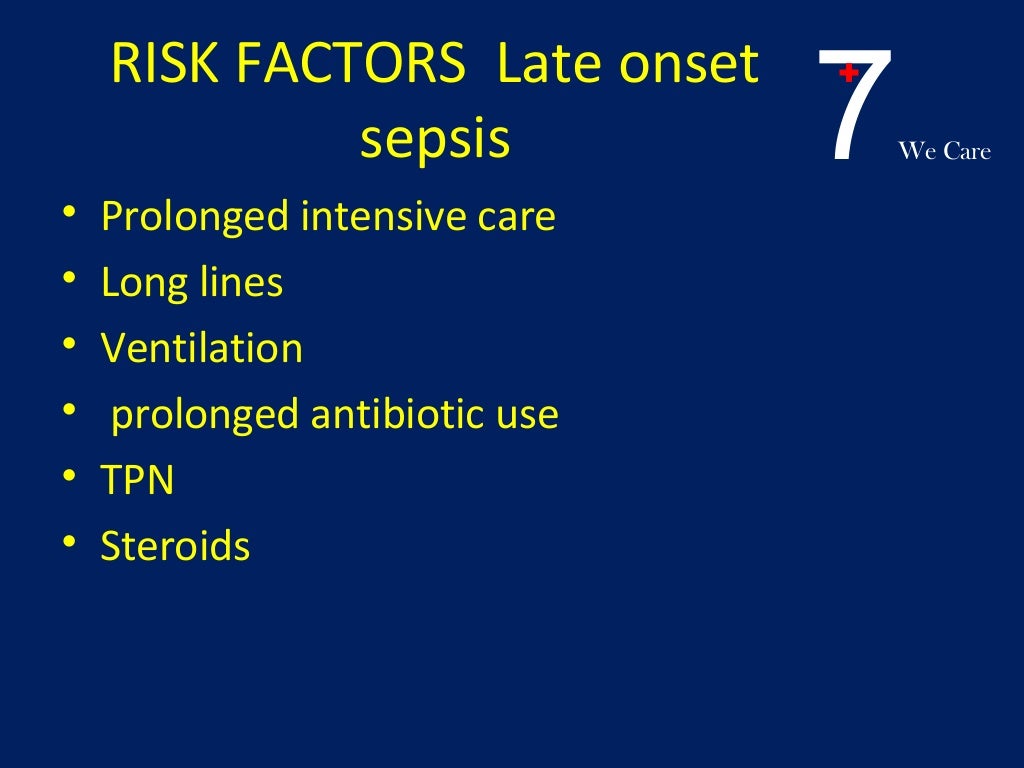
V. Risk Factors: Late onset Sepsis
- Skin or mucosal injury
- Invasive procedures (e.g. Endotracheal Intubation)
- Necrotizing Enterocolitis
- Prolonged antibiotics
- Antacid agents (H2-receptor blockers, Proton Pump Inhibitors)
VI. Causes: Early onset Sepsis (0-7 days of life)
- Common
- Group B Streptococcal Sepsis
- Most common Neonatal Sepsis cause in term infants
- Incidence reduced 80% since Universal GBS Culture and GBS Prophylaxis in U.S.
- Escherichia coli (esp. ECK1)
- Most common Neonatal Sepsis cause in Preterm Infants (<2.5 kg)
- Group B Streptococcal Sepsis
- Other causes
- Listeria monocytogenes
- Rare in the United States (predominant in Spain)
- Streptococcus (other species)
- Enterococcus
- HaemophilusInfluenzae (non-typable)
- Neonatal Herpes Simplex Virus
- Listeria monocytogenes
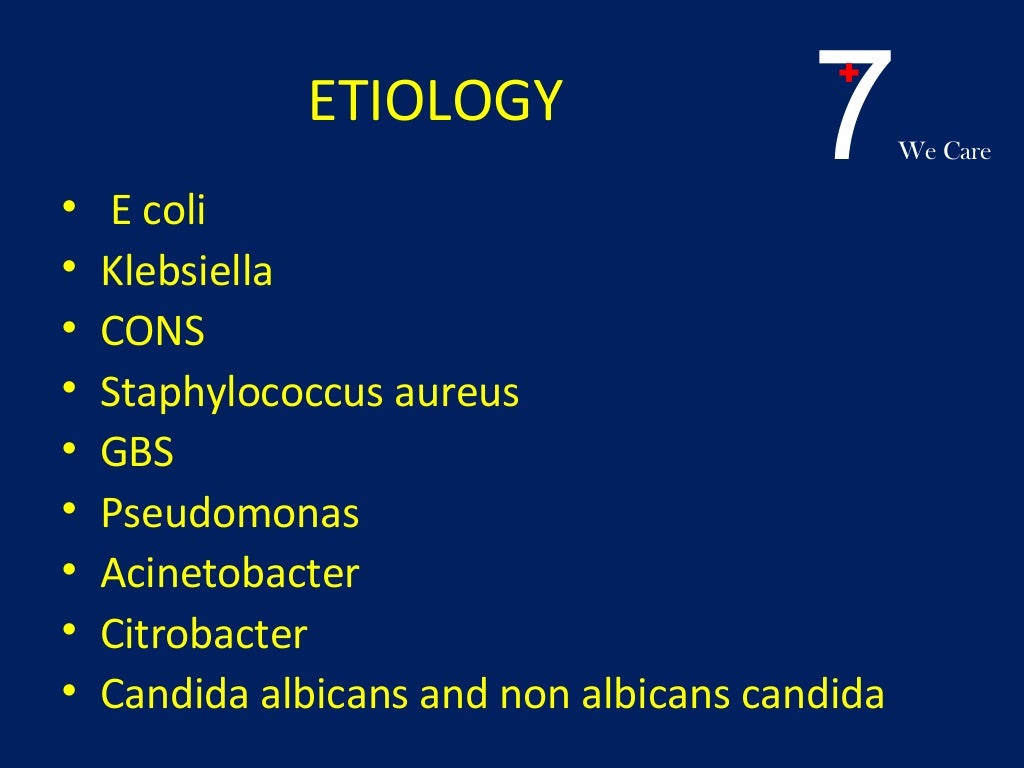
VII. Causes: Late onset Sepsis (7-30 days of life)
- Coagulase-negative staphylococci (Nosocomial)
- Staphylococcus aureus
- Enterococci
- Multi-drug-resistant Gram Negative Rods
- Candida
- Late-onset Group B Streptococcal Sepsis
- Neonatal Herpes Simplex Virus
VIII. History
- See Newborn History
IX. Exam
- See Newborn Exam
- See Pediatric Vital Signs
X. Signs
- Respiratory distress (90%)
- Temperature instability sustained over 1 hour (30%)
- Newborn Temperature < 97 F (36 C)
- Newborn Temperature > 99.6 F (37 C)
- Gastrointestinal symptoms
- Vomiting
- Diarrhea
- Abdominal Distention
- Ileus
- Dehydration signs with poor feeding
- Splenomegaly
- Neurologic
- Cardiovascular
- Skin
XI. Labs
- Bedside Glucose
- Treat Hypoglycemia (Glucose < 40 mg/dl) with D10W 2-4 ml/kg IV
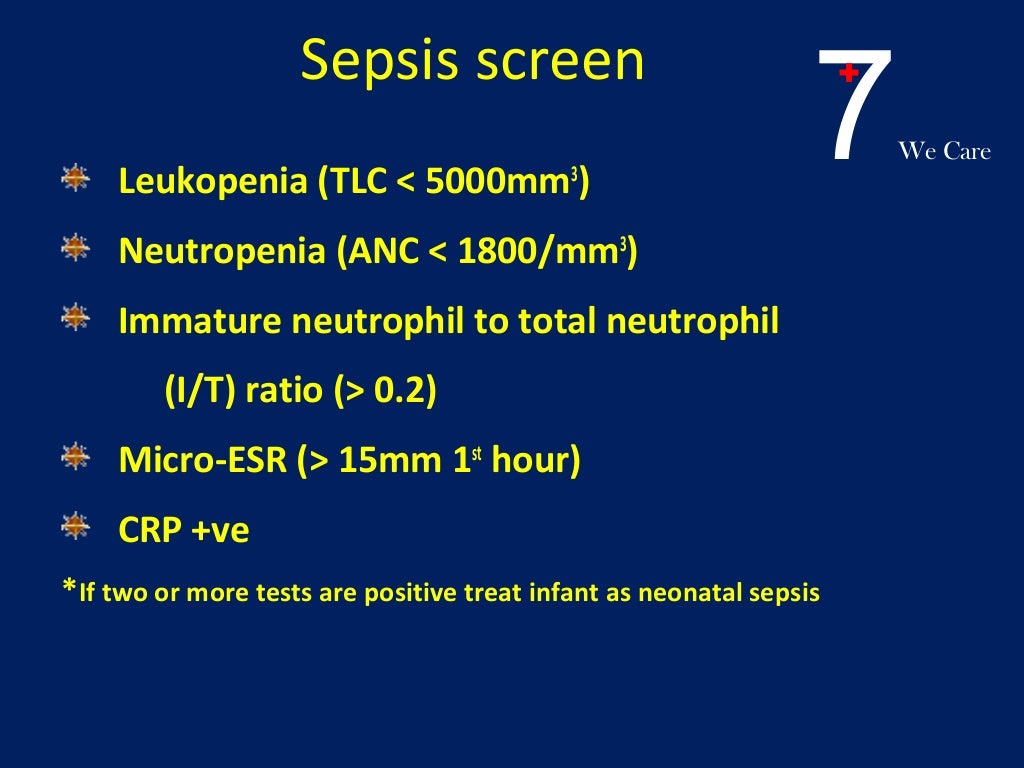
- Complete Blood Count (findings suggestive of Sepsis)
- White Blood Cell Count
- Decreased below 5000 /mm3
- Increased above 25000 /mm3
- Absolute Neutrophil Count (ANC) < 1000 /mm3
- Immature (bands) to total Neutrophil Count ratio > 0.2
- White Blood Cell Count
- C-Reactive Protein
- Reassuring if negative (<10 mg/L) when measured serially in first 24-48 hours (94% NPV)
- Only one elevated C-RP alone is not specific for Neonatal Sepsis
- Basic metabolic panel
- Includes Blood Urea Nitrogen (BUN) and Creatinine
- Blood Culture (positive in 5-10% of Neonatal Sepsis)
- Most important lab to obtain with suspected Neonatal Sepsis
- Lactic Acid
- Arterial Blood Gas (or Venous Blood Gas)
- Indicated for signs or symptoms of Hypoxia
- Lumbar Puncture
- Indications (most cases of suspected Newborn Sepsis)
- Sepsis is considered primary diagnosis
- Blood Culture positive
- Neurologic signs or symptoms
- Specific Tests
- CSF Examination
- CSF Culture
- CSF Antigens
- HSV PCR
- Enterovirus PCR
- Indications (most cases of suspected Newborn Sepsis)
- Urinalysis and Urine Culture
- Indicated for late-onset Neonatal Sepsis
- Not useful in perinatal period (age ❤ days old)
- Consider Urine antigens
- Escherichia coli
- Neisseria Meningitis
- Streptococcal Pneumoniae
- Group B Streptococcus
- Neonatal HSV Testing (if suspected)
- Liver Function Tests
- Coagulation tests such as INR, PTT
- CSF HSV PCR
- Surface culture for HSV (Conjunctiva, mouth, anus, skin lesions)
- Respiratory symptoms during seasonal outbreak times
XII. Differential Diagnosis
XIII. Diagnostics: Electrocardiogram (EKG)
- Indications
- Tachycardia
- Cardiac ausultation findings (e.g. cardiac murmur, gallup, rub)
- Hepatosplenomegaly
- Technique
- Consider obtaing EKG at half speed for easier interpretation
- Expect T Wave Inversion in leads V1 and V2
XIV. Imaging
- Chest XRay
- Indicated in all cases
- Evaluate for Pneumonia, cardiomegaly, Pneumothorax
- Other imaging indicated in specific scenarios
- CT Head
- Indicated for suspected Head Trauma
- Subdural Hematoma may present with findings suggestive of Neonatal Sepsis
- Low grade fever
- Irritability, decreased activity and poor feeding
- CT Head
XV. Management: Stabilization in a septic newborn
- See Newborn Resuscitation
- Endotracheal Intubation
- Indicated in critically ill newborns (RSI not required)
- Oxygenation
- Treat Hypoxia but avoid hyperoxia
- Hyperoxia risks lung and vascular tissue injury due to oxidative stress
- Immediate Intravenous Access
- Umbilical Vein Catheter
- Peripheral IV at scalp vein
- Intraosseous Access
- Indicated for no access after 2 attempts
- Intravenous Fluids
- Initial: 10 ml/kg Normal Saline bolus
- Repeat in 10 ml/kg boluses as needed
- Maximum 20 ml/kg in Preterm Infants (risk of Intracranial Hemorrhage with over-hydration)
- Maximum 40 ml/kg in term infants
- Body Temperature
- Infant should be kept under radiant warmer with abdominal skin probe at 36.5 C (97.7 F)
- Avoid extreme Temperature changes
- Risk of encephalopathic changes, apnea and Temperature dysregulation
- Rewarm hypothermic infants
- Warm blankets
- Warm fluids
- Lower fever
- Antipyretics
- Blood Glucose
- Treat Hypoglycemia (Glucose < 40 mg/dl) with D10W 2-4 ml/kg IV
- Antimicrobials
- Do not delay antibiotics after blood and Urine Cultures to wait for other labs (e.g. Lumbar Puncture)
- Antibiotic selection is described below
- Neonatal HSV management may be indicated (see below)
- Vasopressors
- Dopamine has been first-line Vasopressor for infants with fluid-refractory Septic Shock
- Some expert opinions are to use Norepinephrine (and possibly Epinephrine) instead
- Glucocorticoids
- Indications
- Critically ill newborns (esp. preterm) with fluid/vascopressor refractory hemodynamic instability
- Postulated to treat underlying relative Adrenal Insufficiency
- Dosing
- Hydrocortisone 2 mg/kg
- Indications
- Seizure management
- Correct electrolyte abnormalities
- Endotracheal Intubation
- Indicated for airway management (esp. if Phenobarbital administered)
- Phenobarbital 20 mg/kg IV
- Indicated in intractable Seizures
- Other measures
- Sodium Bicarbonate in Severe Metabolic Acidosis is not typically recommended
XVI. Management: General
- Continue monitoring and antibiotics for 48 to 72 hours
- Indications to continue antibiotics 14 to 21 days
- Symptomatic newborn
- Blood Culture positive
- Discontinue antibiotics and monitoring if
- Blood Cultures negative at 48 to 72 hours and
- No signs of Sepsis on examination
- Indications to continue antibiotics 14 to 21 days
- Signs of Sepsis with negative culture
- Consider Neonatal HSV infection
- Well appearing newborn with isolated fever
- Monitor infant for signs of Sepsis
- Antibiotic indications (contrast with observation only)
- Symptomatic infants
- Asymptomatic infants with >2 risk factors (see above)
XVII. Management: Antibiotics for Early Onset (age <1 week)
- Bacterial spectrum
- Group B Streptococcus
- Escherichia coli
- Klebsiella
- Enterobacter
- Staphylococcus aureus (not common)
- Listeria (rare in United States)
- Protocol: Ampicillin AND Cefotaxime AND Consider Gentamicin
- Antibiotic 1: Ampicillin (Meningitis dose often used empirically)
- Sepsis: 25 mg/kg IV/IM every 8 hours (37 mg/kg every 12 hours if <2 kg)
- Meningitis: 37 mg/kg IV/IM every 8 hours (50 mg/kg every 12 hours if <2 kg)
- Antibiotic 2: Cefotaxime
- Dose: 50 mg/kg/dose IV or IM every 12 hours
- Indicated in Meningitis
- Increased Antibiotic Resistance in Escherichia coli (esp. Preterm Infants)
- Antibiotic 3: Gentamicin (consider)
- Ask pharmacy to assist on dosing and monitoring
- Gestation <30 weeks: 2.5 mg/kg/dose IV/IM q24 hours
- Gestation 30-34 weeks: 2.5 mg/kg/dose IV/IM q18 hours
- Gestation 34-37 weeks: 2.5 mg/kg/dose IV/IM q12 hours
- Gestation >37 weeks: 2.5 mg/kg/dose IV/IM every 8 hours
- Antibiotic 1: Ampicillin (Meningitis dose often used empirically)
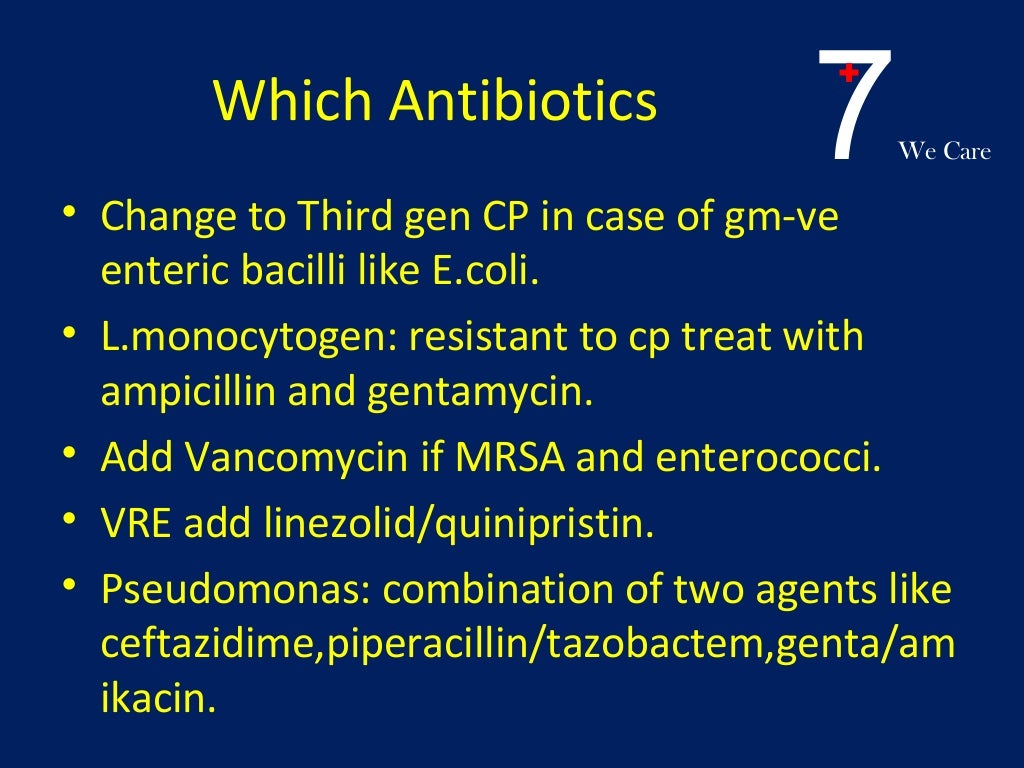
XVIII. Management: Antibiotics for Late Onset (age 1-4 weeks)
- Coverage broadened over early onset Sepsis
- HaemophilusInfluenzae
- Staphylococcus epidermidis
- Antibiotic Dosing for infant over 7 days old
- Ampicillin (the higher dose in possible Meningitis)
- Weight <2 kg: 25-50 mg/kg/dose IV or IM q8 hours
- Weight >2 kg: 25-50 mg/kg/dose IV or IM q6 hours
- Gentamicin
- Ask pharmacy to assist on dosing and monitoring
- Gestation <37 weeks: 2.5 mg/kg/dose IV/IM q12 hours
- Gestation >37 weeks: 2.5 mg/kg/dose IV/IM q8 hours
- Ampicillin (the higher dose in possible Meningitis)
- Primary Protocol 1
- Ampicillin (dosed as above)
- Cefotaxime 50 mg/kg/dose IV or IM q8 hours
- Primary Protocol 2
- Ampicillin (dosed as above)
- Ceftriaxone 75-100 mg/kg/dose IV or IM q24 hours
- Alternative Protocol
- Ampicillin (dosed as above)
- Gentamicin (dosed as above)
- Additional considerations
- Add Vancomycin if MRSA suspected
- Dose: 15 mg/kg IV q12 hours
- Ask pharmacy to assist on dosing and monitoring
- Add Acyclovir if Neonatal HSV suspected
- Dose: 30 mg/kg/day IV divided every 8 hours
- Consider for vesicular rash, Seizure, encephalopathy, transaminitis, DIC
- GBS coverage in severe beta-lactam allergy (Ampicillin allergy)
- Clindamycin (38% GBS resistance)
- Erythromycin (51% GBS resistance)
- Back (2012) Antimicrob Agents Chemother 56(2): 739-42 [PubMed]
- Add Vancomycin if MRSA suspected
XIX. Prevention
- Prolonged Rupture of MembranesGBS Prophylaxis
- Routine Group B Strep Screening in pregnancy (36 weeks)
- NNT 5701 with GBS screening to prevent 1 GBS Sepsis case
- NNT 1191 with GBS treatment to prevent 1 GBS Sepsis case
********************************************************************************














**********************************************************************


































******************************************************************************