Short stature can be a variant of normal growth, or it may indicate a disorder or condition.
SUMMARY
●Short stature is defined as height that is 2 standard deviations (SD) or more below the mean height for children of that sex and chronological age in a given population. This translates to a height that is below the 2.3rd percentile. (See ‘Introduction’ above.)
●The two most common causes of short stature are familial (genetic) short stature and constitutional delay of growth and puberty (CDGP), which are normal variants of growth. These growth patterns often can be distinguished from one another, but some children have features of both.
●Almost any serious systemic disease can cause growth failure (table 2). Systemic disorders or processes that may present with growth failure and/or delayed puberty include undernutrition, glucocorticoid therapy, gastrointestinal disease (especially Crohn disease and celiac disease), and renal disease.
●A variety of genetic syndromes and congenital malformations are associated with short stature. Turner syndrome is particularly important because shortness and/or absent pubertal development may be the presenting feature, with or without other characteristic clinical features (see ‘Turner syndrome’ above). Most of these syndromes can be recognized by characteristic clinical features. These include Noonan, Silver-Russell, and Down syndromes.
Conditions that can underlie short stature include:
- undernutrition, due to a disease or lack of nutrients
- hypothyroidism, leading to a lack of growth hormone
- a tumor in the pituitary gland
- diseases of the lungs, heart, kidneys, liver, or gastrointestinal tract
- conditions that affect the production of collagen and other proteins
- some chronic diseases, such as celiac disease and other inflammatory disorders
Sometimes, an injury to the head during childhood can lead to reduced growth.
A lack of growth hormone can also lead to delayed or absent sexual development.
Rheumatologic diseases, such as arthritis, are linked to short stature. This may happen because of the disease, or as a result of the glucocorticoid treatment, which can affect the release of growth hormone.
Disproportionate short stature (DSS) usually stems from a genetic mutation that affects the development of bone and cartilage and undermines physical growth.
The parents may not have short stature, but they may pass on a condition that is linked to DSS, such as achondroplasia, mucopolysaccharide disease, and spondyloepiphyseal dysplasia (SED).
Types
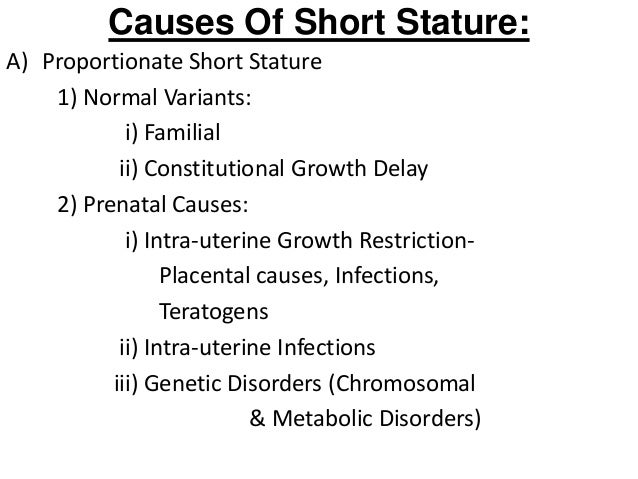
There are different types and causes of short stature, or restricted growth, and they will present differently. Because the range of conditions is so broad, restricted growth can be classified in various ways.
One categorization is:
- Variant restricted growth
- Proportionate short stature (PSS)
- Disproportionate short stature (DSS)
Each of these categories includes a number of types and causes of short stature.
Diagnosis
Some types of short stature can be diagnosed at birth. In other cases, routine visits to a pediatrician should reveal any abnormal growth pattern.
The doctor will record the child’s head circumference, height, and weight.
If the doctor suspects restricted growth, they will carry out a physical examination, look at the child’s medical and family history, and possibly carry out some tests.
These may include:
An x-ray, to assess for problems with bone development
An insulin tolerance test, to check for a deficiency in the growth hormone insulin-like growth factor-1 (IGF-1).
In this test, insulin is injected into a vein, causing blood glucose levels to drop. Normally, this would trigger the pituitary gland to release growth hormone (GH). If GH levels are lower than normal, there may be a GH deficiency.
Other tests include:
- a thyroid-stimulating hormone test, to check for hypothyroidism
- a complete blood count, to test for anemia
- metabolic tests, to assess liver and kidney function
- erythrocyte sedimentation and C-reactive protein tests, to assess for inflammatory bowel disease
- urine tests can check for enzyme deficiency disorders
- tissue transglutinase and immunoglobulin A tests, for celiac disease
- imaging scans, such as an x-ray of the skeleton and the skull or an MRI, can detect problems with the pituitary gland or hypothalamus
- bone marrow or skin biopsies may help confirm conditions associated with short stature
Treatment
Treatment will depend on the cause of the short stature.
If there are signs of malnutrition, the child may need nutritional supplements or treatment for a bowel disorder or other condition that is preventing them from absorbing nutrients.
If growth is restricted or delayed because of a hormonal problem, GH treatment may be necessary.
Pediatric hormone treatment: In children who produce too little GH, a daily injection of hormone treatment may stimulate physical growth later in life. Medications, such as somatropin, may eventually add 4 inches, or 10 centimeters, to adult height.
Adult hormone treatment
: Treatment for adults can help protect against complications, for example, cardiovascular disease and low bone mineral density.
Somatropin, also known as recombinant GH, might be recommended for people who:
- have a severe growth hormone deficiency
- experience impaired quality of life
- are already receiving treatment for another pituitary hormone deficiency
Adult patients generally self-administer daily with an injection.
Adverse effects of somatropin include headache, muscle pain, edema, or fluid retention, problems with eyesight, joint pain, vomiting, and nausea.
The patient may receive treatment to control chronic conditions, such as heart disease, lung disease, and arthritis.
Treatment for DSS
As DSS often stems from a genetic disorder, treatment focuses mainly on the complications.
Some patients with very short legs may undergo leg lengthening. The leg bone is broken and then fixed into a special frame. The frame is adjusted daily to lengthen the bone.
This does not always work, it takes a long time, and there is a risk of complications, including:
- pain
- the bone forming badly or at an inappropriate rate
- infection
- deep vein thrombosis (DVT), a blood clot in a vein
Other possible surgical treatments include:
- use of growth plates, where metal staples are inserted into the ends of long bones where growth takes place, to help bones grow in the right direction
- inserting staples or rods to help the spine form the right shape
- increasing the size of the opening in the bones of the spine to reduce pressure on the spinal cord
Regular monitoring can reduce the risk of complications.
Complications
A person with DSS may experience a number of complications.
These include:
- arthritis later in life
- delayed mobility development
- dental problems
- bowed legs
- hearing problems and otitis media
- hydrocephalus, or too much fluid in the brain cavities
- hunching of the back
- limb problems
- swaying of the back
- narrowing of the channel in the lower spine during adulthood and other spine problem
- sleep apnea
- weight gain
- speech and language problems
Individuals with proportionate short stature (PSS) may have poorly developed organs and pregnancy complications, such as respiratory problems. Delivery will normally be by cesarean section.
************************************************************************
**************************************************************************








*****************************************************************************
INTRODUCTION — Short stature is a term applied to a child whose height is 2 standard deviations (SD) or more below the mean for children of that sex and chronologic age (and ideally of the same racial-ethnic group). This corresponds to a height that is below the 2.3rd percentile. Short stature may be either a variant of normal growth or caused by a disease.
The most common causes of short stature beyond the first year or two of life are familial (genetic) short stature and delayed (constitutional) growth, which are normal, non-pathologic variants of growth.
The goal of the evaluation of a child with short stature is to identify the subset of children with pathologic causes (such as Turner syndrome, inflammatory bowel disease or other underlying systemic disease, or growth hormone deficiency).
The evaluation also assesses the severity of the short stature and likely growth trajectory, to facilitate decisions about intervention, if appropriate.
BIOLOGY OF LINEAR GROWTH — Emerging evidence reveals that normal and pathologic variations in linear growth depend on the balance between proliferation and senescence of chondrocytes at the growth plate. This process is regulated by many systems, including:
●Endocrine mechanisms – Growth hormone (GH), insulin-like growth factor-I (IGF-I), androgens, and thyroid hormone all stimulate chondrogenesis, while glucocorticoids inhibit chondrogenesis. Estrogens promote linear growth by stimulating growth hormone and IGF-I secretion, but also accelerate chondrocyte senescence, leading to fusion of the growth plates and cessation of linear growth [1].
●Proinflammatory cytokines – Some cytokines negatively regulate growth plate function. These are elevated in chronic inflammatory diseases, in which they slow linear growth and also growth plate senescence, which permits catch-up growth after the cytokine effect resolves.
●Paracrine mechanisms – Including fibroblast growth factors, bone morphogenetic proteins, parathyroid hormone-related protein, and others [4].
●Cartilage extracellular matrix – Includes collagens, proteoglycans, and other proteins.
●Intracellular pathways – Chondrocyte transcription factors including SHOX, several SOX genes, and the MAPK signaling pathway.
Together, these effects on the growth plate explain the variations in linear growth observed clinically in health and disease, including normal growth and the pubertal growth spurt, normal variation in height, and “idiopathic” short stature due to polymorphisms in these or other genes and growth delay due to malnutrition, inflammatory disease, or glucocorticoid exposure as well as severe growth failure seen in a variety of skeletal dysplasias (. In some cases, loss-of-function mutations in a gene are associated with short stature, while gain-of-function variants in the same gene are associated with tall stature.
In the clinical setting, these observations explain why growth hormone has variable effects on growth in children with short stature. Growth hormone is highly effective in individuals with growth hormone deficiency, but may also have nonspecific stimulatory effects on the growth plate that can partially compensate for growth problems due to some other molecular defects.
NORMAL VARIANTS OF GROWTH
Familial short stature — Familial or genetic short stature is most often a normal variant . These individuals usually have low-normal height velocity throughout life. The otherwise normal height velocity generally distinguishes these children from those with pathologic causes of short stature. Their bone age is consistent with their chronological age, which helps distinguish them from children with constitutional delay of growth.
Constitutional delay of growth and puberty — Constitutional delay of growth and puberty (CDGP, sometimes called constitutional short stature for prepubertal children) results in childhood short stature but relatively normal adult height. Children with CDGP are usually of normal size at birth.
However, a downward shift in growth rate begins at three to six months of age that is parallel to that seen in most normally growing children in this age group, but tends to be more severe and prolonged. By three or four years of age, children with CDGP usually are growing at a low-normal rate (eg, about 4 to 5 cm/year in preadolescent girls, and 3.5 to 4.5 cm/year in preadolescent boys).
The result is a growth curve that remains below, but parallel to, the third percentile for height. In addition to a low preadolescent height velocity, they tend to have delayed pubertal development. This leads to a marked height discrepancy during the early teenage years compared with their peers, but is followed by catch-up growth when they do enter puberty (figure 2).
The hallmark of CDGP is delayed skeletal age; it is more closely related to the height age (age at which one’s height would be average) than the chronologic age (table 1). For these children and adolescents, height data should be interpreted according to bone age rather than chronological age to accurately reflect height potential.
Because the bone age is delayed, growth typically continues longer than normal, often resulting in adult stature within the normal range. In many cases, there is a family history of delayed growth and puberty in one or both parents (sometimes described as being a “late bloomer”).
Idiopathic short stature — A practical definition of idiopathic short stature (ISS) is a height below 2 standard deviations (SD) of the mean for age, in the absence of any endocrine, metabolic, or other diagnosis. These children have normal (often at the lower limit) height velocity and no biochemical or other evidence for a specific growth retarding condition, which implies normal results for endocrine screening tests, including those for growth hormone deficiency.
Genome-wide studies indicate that the majority of the variation in adult height is explained by several hundred genetic variations, each with a small effect [8]. However, in a small proportion of the population, short stature is caused by specific genetic variations with large effect.
As an example, emerging evidence suggests that mutations in the Short Stature HOmeoboX (SHOX) gene are responsible for 1 to 4 percent of individuals who would otherwise have been classified as having “idiopathic” short statureIn addition to these genetic contributors to ISS, it appears that epigenetic changes may play a role in some cases of ISS. In one study, ISS was associated with increased methylation of two promoter regions for the insulin-like growth factor I (IGF-I) gene; these epigenetic changes are predicted to reduce the individual’s sensitivity to growth hormone [9].
Growth hormone therapy is approved in the United States for children with ISS, which is defined for this purpose by a more stringent threshold for height (below -2.25 SD of the mean, and a predicted adult height is <63 inches [160 cm] for males and <59 inches [150 cm] for girls). However, the use of growth hormone for this group of patients remains controversial. Studies have shown that consumer preferences (family concern) and physician attitudes are important drivers of treatment decisions, independent of patient characteristics [10]. Treatment indications and efficacy are discussed in detail separately.
ISS is a diagnosis of exclusion. The child’s height percentile is below the range predicted by the mid-parental height and the bone age is not delayed, but there is no evidence of underlying genetic, systemic, or endocrine disease [11]. Although this may be a variant of normal growth, patients with this growth pattern warrant monitoring for the possibility of unrecognized underlying disease.
There is ongoing controversy about the nomenclature of ISS. Here, we use the term to refer to non-familial cases (ie, those without patterns of familial short stature). Others consider familial short stature and CDGP to be subcategories of ISS [11,12].
Small for gestational age infants with catch-up growth — Most infants born small for gestational age (SGA) experience catch-up growth by two years of age, sufficient to be within the normal range (length above -2 SD, ie, >2.3rd percentile). Catch-up growth may be delayed in infants who are born preterm in addition to SGA, but often continues into childhood to approach the range predicted by the family’s height. SGA can be caused by maternal, placental, or fetal factors. In many cases these factors (such as intrauterine constraint from a small uterus) are transient and are followed by vigorous catch-up growth during infancy.
About 10 percent of SGA infants, particularly those born with more severe SGA, do not experience catch-up growth to reach the normal range by two years of age. This group of SGA infants can be considered to have a pathologic pattern of growth, so they are discussed later in this topic review.
PATHOLOGIC CAUSES OF GROWTH FAILURE
Systemic disorders with secondary effects on growth — Almost any serious disease can cause growth failure (table 2). The abnormalities of growth and maturation that occur in children with acute or chronic illnesses may result from the primary disease process because of increased energy needs or nutritional deprivation (eg, decreased intake or malabsorption). Growth also may be affected by treatments, such as radiation therapy (a permanent effect), glucocorticoids, stimulants used for attention deficit disorder (ADD), or chemotherapy (mostly transient effects, but may have a small permanent effect if treatment is prolonged [13-16]). Some diseases may cause secondary derangements of the hormones that affect growth.
Diseases or processes that are particularly important causes of growth failure are outlined below. Other disorders that can cause growth failure with weight loss are outlined in a separate topic review. (See “Evaluation of weight loss in infants over six months of age, children, and adolescents”, section on ‘Differential diagnosis’.)
Undernutrition — Insufficient nutrition tends to lead to short stature with a delayed pattern of growth. Under-nutrition can be isolated (eg, caused by inadequate food supply or self-imposed restriction, such as fear of obesity [17]), or it may be a component of an underlying systemic disease that interferes with food intake or absorption, or increases energy needs. The hallmark of under-nutrition is low weight-for-height.
Glucocorticoid therapy — Since glucocorticoids are used for treatment of a variety of diseases, they are a common cause of growth failure in children. The growth failure can develop with or without other symptoms of glucocorticoid excess, known as Cushing syndrome. They suppress growth through several different mechanisms, including interference with endogenous growth hormone secretion and action, bone formation, nitrogen retention, and collagen formation [18]. The growth effects of glucocorticoids are related to the type, dose, and duration of the exposure. If glucocorticoids are discontinued, children usually experience some catch-up growth.
The relative effects of different glucocorticoids on growth are similar, but not identical, to the relative potencies for hypothalamic-pituitary-adrenal axis suppression [19]. Growth impairment is more pronounced with agents with a longer duration of action . It is most pronounced when glucocorticoids are administered daily as compared with an alternate-day regimen [18]. Some inhibition of linear growth occurs even at the doses that are used for physiological replacement (ie, prednisone doses of 3 to 5 mg/m2 per day; approximately 0.075 to 0.125 mg/kg per day), and progressive growth impairment is seen with increasing doses [20]. As an example, in a large series of children with growth failure due to chronic treatment with glucocorticoids for a systemic disease, the mean prednisone-equivalent dose was 0.5 ± 0.6 mg/kg per day [20]. Growth impairment can even occur with prolonged administration of inhaled glucocorticoids during childhood, although the overall effect of these agents on adult height appears to be small [21,22].
Prolonged treatment with systemic glucocorticoids may have persistent effects on growth after therapy is discontinued. In a study of 224 children with cystic fibrosis who previously had been treated for up to four years with either alternate-day prednisone or placebo, mean height after age 18 years (on average six to seven years after cessation of therapy) was significantly lower in boys who had received either high- or low-dose prednisone (170.5 and 170.7 versus 174.6 cm with placebo; p = 0.03) [23]. This effect was most pronounced in boys who had started taking prednisone at six to eight years of age. In contrast, there was no persistent growth impairment in girls treated similarly.
Gastrointestinal disease — Children with growth failure resulting from gastrointestinal disease tend to have a greater deficit in weight than height (ie, they are underweight-for-height) in contrast to those with endocrine disorders, who are often overweight-for-height (see below).
About 30 percent of children with Crohn disease have a decrease in height velocity before the onset of gastrointestinal symptoms [24], and about 10 percent of children with Crohn disease have short stature when the Crohn disease is diagnosed [25,26]. The growth failure is closely related to the inflammatory disease process (mediated by proinflammatory cytokines), as well as decreased food intake, malabsorption, and/orhigh-dose glucocorticoids if used for treatment. Similarly, celiac disease can present with growth failure, especially in younger children [27]. Both of these disorders are important considerations in the evaluation of a child whose linear growth has slowed, particularly if there are gastrointestinal symptoms and/or slow weight gain.
Rheumatologic disease — Childhood rheumatologic diseases, especially systemic juvenile idiopathic arthritis (JIA), are frequently associated with growth retardation [28]. This may be a consequence of the proinflammatory cytokines associated with disease activity and is also caused by the high-dose glucocorticoids that are often used for treatment [29,30]. Common presenting symptoms in JIA are fever, arthralgias, rash, and lymphadenopathy, in addition to growth failure.
Chronic kidney disease — Growth failure is seen in at least one-third of children with chronic kidney disease. The primary causes of growth failure in children with chronic kidney disease are disturbances of growth hormone metabolism and its main mediator, insulin-like growth factor-I (IGF-I). Other factors may include metabolic acidosis, uremia, poor nutrition secondary to dietary restrictions, anorexia of chronic illness, anemia, calcium and phosphorus imbalance, renal osteodystrophy, or use of high-dose glucocorticoids if used for treatment. Affected patients are candidates for growth hormone therapy until renal transplantation, and some of these patients may also benefit from growth hormone therapy after transplantation.
Metabolic acidosis alone can also impair growth, as occurs in children with renal tubular acidosis [31]. Alkali therapy may lead to attainment and maintenance of normal stature .
Cancer — Children with cancer may grow poorly before diagnosis because of poor food intake, nausea, vomiting, and increased caloric utilization. After diagnosis, anorexia, nausea, and vomiting induced by chemotherapy and radiotherapy also can contribute to impaired growth. These effects often subside within one to two years of initiating treatment, and some children then have catch-up growth [32,33].
Late growth failure is common in children who received cranial radiotherapy because it can damage the hypothalamus and cause insufficiency of one or more hormones from the pituitary, including growth hormone, gonadotropins, and thyroid stimulating hormone (TSH) [34-38]. In younger children, especially girls, cranial radiotherapy can cause precocious puberty and adult short stature. Primary hypothyroidism also can occur if the thyroid gland was in the radiation field. Spinal irradiation may result in slow growth of the spine with relative preservation of normal limb growth.
Pulmonary disease — Cystic fibrosis is both a pulmonary and gastrointestinal disease. Growth failure in children with this disorder may be caused by multiple mechanisms, including poor food intake, maldigestion or malabsorption, chronic infection, and increased energy requirements (work of breathing)
Immune deficiencies also may present with pulmonary symptoms and/or growth failure.
Asthma has been associated with a deceleration of height velocity, which is most pronounced with severe disease. Growth failure in children with asthma is usually due to treatment with glucocorticoids, including inhaled glucocorticoids.
Cardiac disease — Growth failure is common in children with severe heart disease of any cause. The major pathogenetic factors are thought to be anorexia and increased basal energy requirements [40]. Occasionally, growth failure is the presenting feature of the heart disease.
Immunologic disease — Human immunodeficiency virus (HIV) infection is associated with growth failure. Mechanisms include anorexia, malabsorption, diarrhea, severe infections, and failure of one or more organ systems.
Growth failure also can occur with other immunological deficiencies such as common variable immunodeficiency or severe combined immunodeficiency syndrome. As with HIV infection, multiple factors are probably involved.
Metabolic diseases — Growth failure is common in children and adolescents with many of the inborn disorders of metabolism. Among acquired metabolic diseases, the most common is type 1 diabetes mellitus. In the past, type 1 diabetes mellitus was an important cause of short stature and attenuated growth because of caloric deficit resulting from severe glucosuria [42]. However, it is now rare because of improvements in therapy. Children with type 1 diabetes have some decrease in IGF-I production or action, and there is a negative correlation between hemoglobin A1C percent (as an index of metabolic control) and adult height [43,44]. Nonetheless, in children with fair to good metabolic control, growth and adult height are usually within normal ranges. Occasionally, children with diabetes and very poor glycemic control develop Mauriac syndrome, characterized by attenuated linear growth, and delayed puberty, hepatomegaly, and Cushingoid features.
Any disorder associated with vitamin D deficiency or decreased vitamin D action can cause hypophosphatemia and rickets; rickets is characterized by abnormal epiphyseal development, bowing of the extremities, and diminished growth. Vitamin D deficiency in the absence of rickets does not seem to affect linear growth.
Endocrine causes of growth failure — Primary endocrine disorders with effects on growth are uncommon but are important to identify because they can be treated (table 2). In general, these disorders are characterized by excessive weight for height. They should be considered in any child with markedly reduced height velocity, and especially in those with other pituitary disorders, brain tumors, optic nerve hypoplasia (also known as septo-optic dysplasia), midline brain and facial defects, neonatal hypoglycemia, history of cranial irradiation, or a familial pattern of growth hormone deficiency [45]. Any patient with an abnormality of one pituitary hormone (central hypothyroidism, Cushing disease, or growth hormone deficiency) should be evaluated for other pituitary hormone deficiencies.
Cushing syndrome — Cushing syndrome is caused by excessive glucocorticoids and is characterized by the combination of weight gain and growth retardation, resulting in excessive weight-for-height (figure 3) [46-48].
Endogenous Cushing syndrome (caused by excessive endogenous production of cortisol) is rare in children. The most common cause is a corticotropin (ACTH)-secreting pituitary adenoma (Cushing disease) [46,48,49]. The syndrome also may be caused by an adrenal adenoma, especially in younger children. In one series of children with endogenous Cushing syndrome, growth retardation was common (83 percent), but most patients had bone age within normal limits at diagnosis [46]. Other key clinical features are central obesity, suprascapular fat pad (“buffalo hump”), abdominal striae, hirsutism, acne, and neuropsychological symptoms [48]. The best tests to establish the diagnosis are a 24-hour urine collection for free cortisol (and creatinine), or a dexamethasone suppression test. Measurements of serum cortisol are not reliable screening tests, unless performed late at night.
Exogenous sources of glucocorticoids (eg, due to glucocorticoid therapy for asthma or inflammatory bowel disease) are a much more common cause of Cushing syndrome.
Hypothyroidism — Growth failure is a well-recognized consequence of hypothyroidism during childhood and may be the presenting feature. The bone age is usually delayed; as a result, many children with hypothyroidism have a reasonably normal growth potential once the disorder is identified and treated. The evaluation should include measurements of both TSH and free thyroxine to allow detection of both primary and central hypothyroidism. Measurement of serum TSH alone will not detect central hypothyroidism as it can be low, normal, or even slightly elevated.
Growth hormone deficiency — Growth hormone deficiency usually results from deficiency of growth hormone-releasing hormone (GHRH). It can also be caused by sellar and parasellar tumors (eg, craniopharyngioma [50]) that destroy the pituitary gland itself, in which case there may be deficiencies of multiple hormones produced by the anterior pituitary. Children with growth hormone deficiency can have striking catch-up growth during growth hormone replacement therapy [51]. Children with a sellar or parasellar tumor that causes growth hormone deficiency occasionally experience rapid catch-up growth after surgical resection of the tumor without growth hormone treatment; this phenomenon is known as “growth without growth hormone” and is not fully understood [52,53]. A rare cause of growth hormone deficiency is an inactivating mutation of the GHRH receptor that is inherited in an autosomal recessive manner [54].
If growth hormone deficiency is congenital and complete, the diagnosis is relatively easy to confirm. Affected children present with severe postnatal growth failure, delayed bone age, and very low serum concentrations of growth hormone, IGF-I, and IGF-binding protein-3 (IGFBP-3, the major circulating binding protein for IGF-I) [45]. Additional findings are hypoglycemia, prolonged jaundice, and micropenis, especially if gonadotropins are deficient as well.
In children with less severe growth failure, whose height may still be within the normal range for age, the decision to undertake detailed testing should be based on strict auxological criteria. It is therefore mandatory to obtain accurate serial measurements of height. Any evidence of central nervous system disease or other anterior pituitary hormone deficiencies should lead to measurement of IGF-I and provocative testing of growth hormone (growth hormone stimulation tests). These provocative tests are not definitive but can be a valuable diagnostic tool when combined with auxological and bone age data and measurements of IGF-I and IGFBP-3.
Congenital growth hormone insensitivity is a very rare disorder characterized by high serum growth hormone concentrations with low serum IGF-I and IGFBP-3 concentrations [45]. In its complete form, this condition is called Laron-type dwarfism (complete growth hormone insensitivity)
Sexual precocity — Several conditions are associated with increased secretion of gonadal steroids (estradiol in girls and testosterone in boys), which have two consequences. One is sexual precocity. The other is accelerated epiphyseal development, which causes rapid childhood growth but more rapid advancement of bone age. As a result, height age is advanced compared with chronologic age, but it lags behind the markedly accelerated bone age. If their growth is not halted, these tall children will be short adults because early epiphyseal closure stops linear growth prematurely.
There are two types of sexual precocity:
●Gonadotropin-dependent precocious puberty (GDPP), also known as central (or true) precocious puberty, refers to the early occurrence of normal puberty. Precocious puberty historically had been defined as sexual development in girls before the age of eight years and in boys before the age of nine years; however, data for girls, particularly black girls, indicate that the age of onset of normal puberty is younger [56-58]. The hallmarks of precocious puberty are accelerated growth and advanced bone age, plus breast development in girls and penile enlargement and sexual hair growth in boys [59]. The pattern of secretion of pituitary gonadotropins and gonadal sex steroids is normal but early.
Genetic diseases with primary effects on growth — Several genetic disorders have prominent effects on growth. These disorders occasionally present with short stature as the initial clinical manifestation. Many other genetic disorders, such as Down syndrome, include short stature but are not listed here because stature is not a primary identifying characteristic.
Turner syndrome — Turner syndrome is an important consideration in girls with short stature and especially growth failure, because shortness may be the presenting feature of the syndrome; other physical abnormalities are variably expressed (table 3). Virtually all girls with Turner syndrome have short stature, with an average adult height about 20 cm shorter than predicted by the mid-parental height. In addition, affected patients usually have absent or very delayed pubertal development and may have a square “shield” chest, webbed neck, cubitus valgus (increased carrying angle of the arm), genu valgum (inward tilting knees), shortened fourth metacarpals, and Madelung deformity of the forearm (picture 1 and image 1). A Madelung deformity is a growth disturbance in the distal radial epiphysis that results in volar and ulnar tilted distal radial articular surface, volar translation of the hand and wrist, and a dorsally prominent distal ulna and wrist pain; this condition is sometimes termed “bayonet wrist”. Prompt diagnosis of Turner Syndrome is important because of associated cardiovascular, renal, and endocrine abnormalities, which may require treatment, including growth hormone therapy.
SHOX mutations — Mutations in the Short Stature HOmeoboX (SHOX)-containing gene on the X chromosome cause a syndrome in which the primary manifestation is short stature, which tends to be more severe in girls (MIM #300582). In addition to short stature, individuals with this mutation tend to have shorter forearms and lower legs (with reductions in arm span and leg length compared with trunk), Madelung deformity of the forearm (focal dysplasia of the distal radial physis) (picture 1 and image 1), cubitus valgus (increased carrying angle of the arm), high arched palate, and muscular hypertrophy (reflected as a short, stocky appearance), as compared with those with idiopathic short stature but no SHOX mutation [62]. These skeletal abnormalities are similar to those seen in many patients with Turner syndrome.
SHOX mutations are present in approximately 1 to 4 percent of patients who would otherwise have been classified as having “idiopathic” short stature [62-64]. The SHOX gene is found in the pseudoautosomal region of the X and Y chromosomes, and also is responsible for the short stature and skeletal deformities associated with Turner syndrome, Leri-Weill dyschondrosteosis, and Langer mesomelic dysplasia [63,65-68] . Growth hormone treatment is effective in increasing linear growth in patients with isolated SHOX deficiency [69-71].
Prader-Willi syndrome — Prader-Willi syndrome (PWS) (MIM #176270) is the most common syndromic form of obesity. Obesity and hyperphagia typically develop during early childhood and can be severe. Other common clinical characteristics are hypotonia and feeding problems during infancy, developmental delay, and hypogonadism. Short stature is common but may not develop until late childhood when the child fails to undergo a pubertal growth spurt. Treatment with growth hormone improves linear growth and body composition.
Noonan syndrome — Noonan syndrome (MIM #163950) is a relatively common autosomal dominant disorder that is associated with short stature and congenital heart disease (CHD), most often pulmonic stenosis. It is clinically and genetically heterogeneous. It is clinically heterogeneous and can present at any age. The most consistent clinical features are widely spaced eyes and low-set ears (>80 percent), short stature (>70 percent), and pulmonic stenosis (approximately 50 percent) [72]. Children with Noonan syndrome may present with short stature, a murmur indicating CHD, or delayed speech or motor milestones. Short stature associated with Noonan syndrome can be treated effectively with growth hormone. This disorder is discussed in detail in a separate topic review. (See “Noonan syndrome”.)
Silver-Russell syndrome — Silver-Russell syndrome (MIM #180860, also known as Russell-Silver syndrome and Russell-Silver dwarfism) is characterized by severe intrauterine growth restriction and postnatal growth retardation with a prominent forehead, triangular face, downturned corners of the mouth, and body asymmetry (hemihypertrophy) [73,74]. The facial features tend to become less obvious with age. The majority of infants have feeding difficulties, and mild developmental delay is seen in about one-third of subjects [75]. In about 60 percent of subjects, the syndrome is associated with epigenetic alterations involving either hypomethylation of an imprinting control region that regulates expression of the insulin-like growth factor-2 (IGF-2) gene and others on chromosome 11p15.5. IGF-2 is known to have important effects on growth, especially during fetal development. About 10 percent of cases are caused by maternal uniparental disomy of chromosome 7 [76]. Accordingly, one study describes severe pre- and post-natal growth restriction in four members of the same family with clinical features of Silver-Russell syndrome, due to a paternally-inherited mutation in the IGF-2 gene [77].
A few reports suggest modest efficacy of growth hormone (GH) treatment of individuals with Silver-Russell syndrome; the growth hormone was given based on the indication for individuals born small for gestational age [77-81]. When growth hormone was started at a young age, the mean adult height in treated subjects was -1.3 standard deviations (SD) [78], compared with an adult height of -4.2 to -2.9 SD in untreated subjects with this disorder [78,82]. In a separate large study, mean adult height in GH-treated subjects was -2.17 SD, despite a mean total height gain of 1.3 SD [83]. A comparison group of children born SGA, but without Silver-Russell syndrome, had somewhat better adult height outcomes (mean –1.65 SD). Of note, individuals with the hypomethylation defect tend to have inappropriately high levels of IGF-I and IGFBP-3, suggesting a reduced sensitivity to IGF-I [75,84].
Skeletal dysplasias — Skeletal dysplasias associated with short stature are caused by inherited defects in cartilage/bone development and are often associated with disproportionate short stature (with limbs disproportionately short for the trunk, or vice versa). Some present prenatally and are detected on prenatal ultrasound, whereas others present during childhood with short stature. These disorders should be suspected in a child presenting with short stature and bone deformities, recurrent fractures, or abnormal findings on radiographs (eg, enchondromas, bowing or shortening of the long bones, vertebral defects, or rib abnormalities).
There are a variety of types, with very variable phenotypes, including achondroplasia, hypochondroplasia, spondyloepiphysial dysplasia, and osteogenesis imperfecta. In one study, subtle skeletal dysplasias were found in 18.5 percent of patients previously labeled as either idiopathic short stature (ISS) or having been born small for gestational age (SGA) [85]. The most common forms were dyschondrosteosis (due to SHOXmutations in 61.5 percent of those undergoing genetic testing) and hypochondroplasia (due to FGFR mutations in 25 percent of those subjects undergoing genetic testing). These disorders were especially prevalent among those with parents who are also very short.
SUMMARY
●Short stature is defined as height that is 2 standard deviations (SD) or more below the mean height for children of that sex and chronological age in a given population. This translates to a height that is below the 2.3rd percentile. (See ‘Introduction’ above.)
●The two most common causes of short stature are familial (genetic) short stature and constitutional delay of growth and puberty (CDGP), which are normal variants of growth. These growth patterns often can be distinguished from one another, but some children have features of both.
●Almost any serious systemic disease can cause growth failure (table 2). Systemic disorders or processes that may present with growth failure and/or delayed puberty include undernutrition, glucocorticoid therapy, gastrointestinal disease (especially Crohn disease and celiac disease), and renal disease.
●A variety of genetic syndromes and congenital malformations are associated with short stature. Turner syndrome is particularly important because shortness and/or absent pubertal development may be the presenting feature, with or without other characteristic clinical features (see ‘Turner syndrome’ above). Most of these syndromes can be recognized by characteristic clinical features. These include Noonan, Silver-Russell, and Down syndromes.
*******************************************************************************************************************************************************************